Introduction. Umbilical cord blood transplantation (UCBT) is an efficacious therapeutic intervention for pediatric acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). However, contention persists regarding how best to achieve long-term relapse-free survival (RFS). Differences in clinical practice can be attributed to an incompletely understood interplay between graft-versus-leukemia (GvL) effect and graft-versus-host disease (GvHD), as well as an incomplete understanding of how UCBTs differ from those of other stem cell sources. Human leukocyte antigen (HLA) matching is a critical determinant of post-transplant outcome, but factors such as GvHD prophylaxis and total body irradiation (TBI) usage also play a key role.
Objective. To use unsupervised clustering algorithms to examine the interplay between HLA matching, immunosuppressive regimens, and conditioning factors with greater power than that conferred by conventional multivariate regression analyses.
Methodology. Data pertaining to UCBTs performed for pediatric ALL (n = 908) and AML (n = 417) between 2004 and 2022 was obtained from the Eurocord/EBMT registry. ALL and AML UCBTs were separately subjected to a partitioning around medoids clustering algorithm, which identified k = 15 ALL clusters and k = 11 AML clusters. These clusters were used to form hypotheses for post-hoc testing, which were tested using Kaplan-Meier and competing risks analyses.
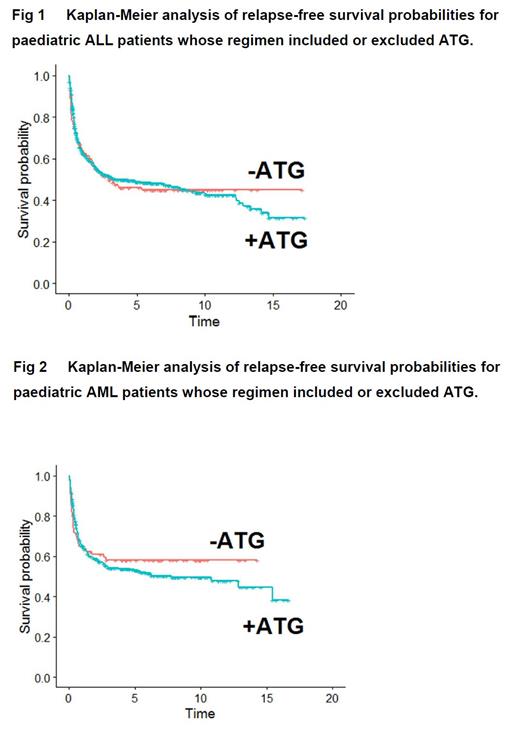
Results. Clusters of both diseases were frequently divided by usage of ATG, which was administered in 77% of 8/8 ABCDR matched UCBTs. ALL and AML patients who did not receive ATG experienced greater RFS than recipients of ATG, and this appeared to be driven by elimination of relapse mortality in the late (≥5 year) post-transplant setting (Figs 1-2). ALL clusters were frequently divided by use of total body irradiation (TBI), and those featuring TBI regimens conferred RFS comparable or superior to non-TBI regimens; this appeared to be driven by a reduction in relapse mortality within the first three years post-UCBT (P = 0.007). In AML but not ALL, both HLA-C and KIR match levels appeared to be relevant (P = 0.04), despite typing only having been performed for 70% and 24% of AML UCBTs, respectively. Patients receiving a 7/8 ABCDR-matched graft with a single HLA-C mismatch experienced significantly poorer RFS than 8/8 matched UCBTs (P = 0.04), but a concomitant single co-mismatch at HLA-A or HLA-B appeared to restore RFS to levels comparable to 8/8 matched grafts.
Conclusions. ATG is over-used in ALL and AML patient-graft pairings where risk of non-relapse mortality (NRM) is low, and this may be creating an avoidable risk of relapse. The conflicting results in published literature may be explained by follow-up time, as the effect does not become apparent until 5 years post-UCBT and many studies do not follow patients beyond this. Incorporation of TBI into ALL myeloablative regimens prevents relapse mortality in the early to mid-post UCBT setting, and this effect was independent of HLA matching. These findings align with the known genetic and biological determinants of these diseases and redouble the importance of typing at HLA-C in AML; administration of TBI in ALL; and a measured approach to the usage of ATG.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal